BOSTON — March 14, 2016 — “We applaud the Governor and the Legislature for their swift and thoughtful action to help combat the ongoing opioid crisis in Massachusetts. Health plans can and should play a meaningful role in what is a community-wide problem and we are honored that our program is part of the effort. We look forward to continuing to work with the Governor and Legislature to further tackle this epidemic in the years to come.” Andrew Dreyfus, Blue Cross CEO.
-------------------------------------------------------------------------------------------------
Background on Blue Cross’ Pain Management Safety Program
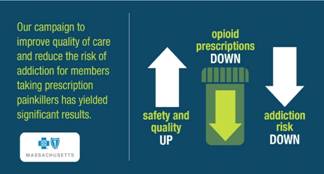
In 2012, we created a first-in-the-nation Pain Management Safety Program in an effort to reduce the risk of addiction to opioid-based painkillers while ensuring our members get the best care.We conceived our program with the help of outside experts in pain management, primary care and addiction services. The result is an evidenced-based program that offers affordable, accessible and appropriate pain care; helps reduce risk of member addiction and diversion of prescription drugs. As is the case with the bill passed today, our program has always included important protections for members with cancer diagnoses.
|
Since its inception, our Pain Management Safety Program has:
|
|
Helping members get the care they need
We know that our responsibility does not end with reducing the supply of drugs, which is why we are also committed to finding new and innovative ways to treat our members and provide them with the care they need. For example:
- We have a physician expert in addiction medicine that helps guide our efforts and works with the providers in our network, our customers and our members.
- In 2014, we launched our REACH Program. Members who chose to participate have access to a series of traditional and non-traditional treatments and interventions including: 24/7 access to a care manager; peer counseling; living skills training; family support groups; co-pay assistance; and even transportation to and from health care appointments.
- Last year, we removed barriers for behavioral health admissions from emergency rooms. If a physician believes that an admission is necessary, our member is admitted. And through an agreement with two of our state’s largest detox and addiction providers, we contact our members while they are still in these facilities to identify potential gaps in their care and ensure that they understand their treatment plans.
- We continue to educate consumers and recently produced a video that powerfully illustrates the problem and offers hope and resources to those who may be suffering from addiction.
- We cover drugs such as narcan and suboxone to ensure our members with substance use disorders have access to medication assisted therapies.
About Blue Cross Blue Shield of Massachusetts
Blue Cross Blue Shield of Massachusetts (www.bluecrossma.com) is a community-focused, tax-paying, not-for-profit health plan headquartered in Boston. We are the trusted health plan for more than 30,000 Massachusetts employers and are committed to working with others in a spirit of shared responsibility to make quality health care affordable. Consistent with our corporate promise to always put our 2.8 million members first, we are rated among the nation's best health plans for member satisfaction and quality. Connect with us on Facebook, Twitter, YouTube and LinkedIn.