Visit Blue Cross' new health news site, Coverage, for compelling original reporting on health and wellness issues. Sign up to get our weekly headlines in your inbox!
Pay attention to your body, and do not be afraid to get a mammogram.
That’s what breast cancer survivor Rebecca Seago-Coyle constantly tells other women.
“I was 34 years old and noticed a lump on my breast,” recalls Seago-Coyle of Bend, Ore., above, now the editorial and community director for Patient Power, a cancer patient and cancer survivor support organization in Seattle, Wash. “I decided to get screened. My left breast came back showing certain abnormalities and that led to a biopsy that came back positive for breast cancer."
Recommended treatment varies according to diagnosis, genetics and family history. However, advances in technology and treatment have made early screening more important than ever, clinicians say.
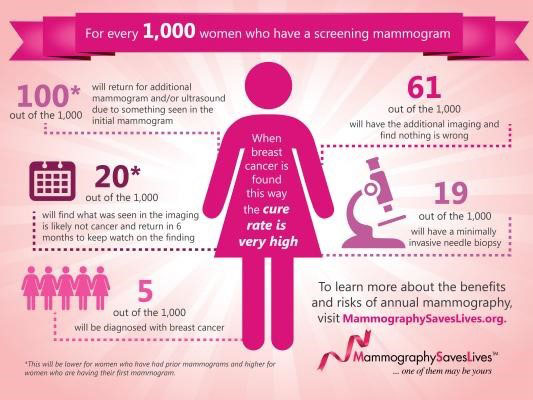
“Breast cancer is the most common cancer, with 1 in 8 women expected to develop it,” said Beth Israel Deaconess Medical Center’s chief of breast imaging and co-director of the Linsey Breast Care Center Dr. Tejas S. Mehta, “Early detection will and does save people’s lives. In combination with advances in treatment, the advent of screening mammography has helped reduce the mortality rate by 35-40% for breast cancer patients.”
In 2015, there were an estimated 231,840 new cases diagnosed, according to Susan G. Komen.
Regular screening
Most experts recommend mammogram screening every other year starting at age 50 for women with average breast cancer risk, even if they have no symptoms
“Symptoms have nothing to do with this as breast cancer is not revealed through any particular symptom,” noted Dr. Katherine Dallow, vice president and medical director at Blue Cross Blue Shield of Massachusetts.
“Cancer is asymptomatic and most women diagnosed with breast cancer do not have a family history of breast cancer,” Mehta agreed. “The guidelines created for providers are speaking to the average risk woman. So if we are looking at someone who is higher risk, not only should they be screened with mammography but with MRIs.”
Any woman who is at high risk (for example, with a family history of cancer), or who has concerns about the benefits and risks of mammograms, should consult her primary care provider about whether screening before age 50 is appropriate.
“There are many different guidelines care providers use to inform patient’s decisions,” Mehta said. “The American College of Radiology, the U.S. Preventative Taskforce, American Cancer Society, American College of OBGYN develop guidelines for providers to follow, and because different providers follow different guidelines, patients may become confused as to when they should get their mammograms. But make no mistake, most breast cancer detection occurs through screening mammography than any other method.”
Clinicians recommend any woman who finds a lump in her breast schedule an appointment with a doctor and a mammogram. They note few lumps are cancerous. “Finding a lump in your breast just means you need to schedule a mammogram and get evaluated,” Dallow said.
Safe and sophisticated
Mammography is highly regulated by the Food and Drug Administration, the Mammography Quality and Standards Act and other governing organizations like the American College of Radiology. Mammograms use very small doses of radiation and the risk of harm is very low.
“To put it in perspective, the dose of radiation is lower than that of a chest x-ray,” Mehta said.
“When a provider recommends getting screened, it indicates the risks outweigh the benefit and it is deemed to be safe,” Dallow said, adding that under the Affordable Care Act, insured patients have no copay for the mammogram. “The mammogram is covered as a preventive benefit so getting it involves no cost.”
Researchers are examining whether new technology such as tomosynthesis, or three-dimensional mammography, may improve diagnosis.
“A 3-D mammography allows us to peel away at the layers and see the breast tissue better,“ Mehta said, noting studies are underway. “Now, because of some skepticism about patient outcomes, people are being randomized between 2-D and 3-D. These patients are tracked to see if 3-D mammography really changes the long-term survival rate and outcome for them.”
Clinicians and patients agree: Do not hesitate to get a mammogram.
“You know yourself better than anybody,” Seago-Coyle said. “If you feel that something is not quite right or not normal, regardless of your age, and you have a family history of cancer, talk to your doctor and don’t prolong getting screened. It could save your life.”