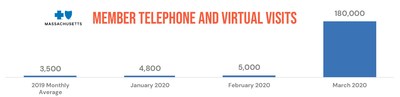
BOSTON, April 13, 2020 /PRNewswire/ -- Blue Cross Blue Shield of Massachusetts ("Blue Cross") announced today that it has processed 250,000 telehealth claims since changing its policy to both expand coverage for telephone and virtual visits and reimburse them at the same rate as in-person visits during the COVID-19 state of emergency. The March telehealth claims figure is a 3600% increase over February and a 5100% increase over the monthly average for 2019.
Blue Cross is working at full capacity to process claims to the health care delivery system. In March alone, Blue Cross made payments of nearly $800 million to physician and hospitals, including more than 50,000 new claims for COVID-19 testing and care, totaling approximately $10 million.
Additionally, Blue Cross is accelerating payments to provider groups participating in its Alternative Quality Contract (AQC). Under normal circumstances, these incentive payments would have been made in late 2020 or early 2021. This direct financial support is intended to assist providers with the financial pressures associated with the COVID-19 public health emergency.
"We want to do everything we can to support our members, employer customers, and clinician partners under these extraordinary circumstances," said Andrew Dreyfus, president and CEO of Blue Cross. "Telehealth is a critical resource - it's allowing clinicians to continue caring for their patients, and it's also helping limit the spread of contagion by keeping people out of emergency rooms and doctors' offices unless absolutely necessary."
In support of Governor Charlie Baker's order to expand access to physician services, Blue Cross has also developed a new expedited credentialing and enrollment process for practitioners, designed to speed health plan approval within 72 hours. The Public Health Emergency Provider Credentialing and Enrollment Process includes a simplified, one-page application and essential documentation requirements consistent with conditions for licensure with the Massachusetts Board of Registration in Medicine. Approval under this expedited process is time-limited and in effect for the duration of the Massachusetts public health emergency.
"Simplifying this process to remove potential barriers to providing access to hospital-based clinicians will help meet the growing demand for care during this pandemic," said Bruce Nash, MD, chief physician executive and senior vice president of health and medical management at Blue Cross. "We want clinicians to be able to focus on patients rather than paperwork."
The expedited process supports clinicians responding to this crisis, including behavioral health practitioners seeking to provide services via telemedicine (phone or video) to Blue Cross members during the public health emergency.
Blue Cross has taken several additional steps to ensure that our clinician partners can focus on the care of our members during the COVID-19 emergency. These steps include:
- Removing administrative barriers, such as prior authorizations and referrals, for medically appropriate testing, counseling, vaccines (when available) and treatment for COVID-19, consistent with the Centers for Disease Control and Massachusetts Department of Public Health guidelines.
- Covering all medically necessary covered services via phone (telephonic) or virtually (telehealth) with in-network providers at no cost to members, and reimbursing these visits at the same rate as face-to-face care for any provider, for both medical and behavioral health care, as long as they meet clinical standards, for the entire period of the Massachusetts public health emergency. Telehealth is allowing many clinicians to continue providing care and services to patients remotely throughout the pandemic. In fact, the latest data from a Blue Cross/MassINC tracking poll found a more than 200% rise in the use of telemedicine in recent weeks.
- Removing prior authorization requirements and moving to a notification-only requirement for inpatient levels of care including Acute, Long Term Acute (LTAC), Acute and Subacute Rehabilitation (Rehab), and Skilled Nursing Facility (SNF) admissions. Medical necessity reviews will not be performed for these inpatient levels of care through June 23, 2020. This is being done to facilitate inpatient capacity across the health care system during the state of emergency.
- Suspending prior authorization requirements for scheduled surgeries or admissions at hospitals (notification only, to coordinate patient care management and ensure that Blue Cross members are protected from balance billing).
- Suspending concurrent and retrospective review for hospital inpatient services.
- Ensuring prompt, efficient payment of claims: Blue Cross is committed to meeting the state's prompt pay law requirements during this time and is working at full capacity to ensure we process claims quickly.
- Publishing and sharing a detailed guide clearly outlining Blue Cross' coding and billing policies.
For more information on how Blue Cross is responding to the COVID-19 public health emergency, please click here.
About Blue Cross Blue Shield of Massachusetts
Blue Cross Blue Shield of Massachusetts (www.bluecrossma.com) is a community-focused, tax-paying, not-for-profit health plan headquartered in Boston. We are committed to the relentless pursuit of quality, affordable health care with an unparalleled consumer experience. Consistent with our promise to always put our members first, we are rated among the nation's best health plans for member satisfaction and quality. Connect with us on Facebook, Twitter, YouTube, and LinkedIn.
SOURCE Blue Cross Blue Shield of Massachusetts