BOSTON, MA – October 30, 2014 – An independent study released today in the New England Journal of Medicine (NEJM) shows that the Blue Cross Blue Shield of Massachusetts (Blue Cross) Alternative Quality Contract (AQC) has improved the quality of patient care and lowered costs in the four years since it was first implemented.
Key Study Findings
The study – by researchers at Harvard Medical School and funded by the Commonwealth Fund and the National Institute on Aging – compares Blue Cross members with a Primary Care Physician (PCP) in an AQC contract with a control group comprised of commercially-insured individuals across eight northeastern states (Connecticut, Maine, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island and Vermont).
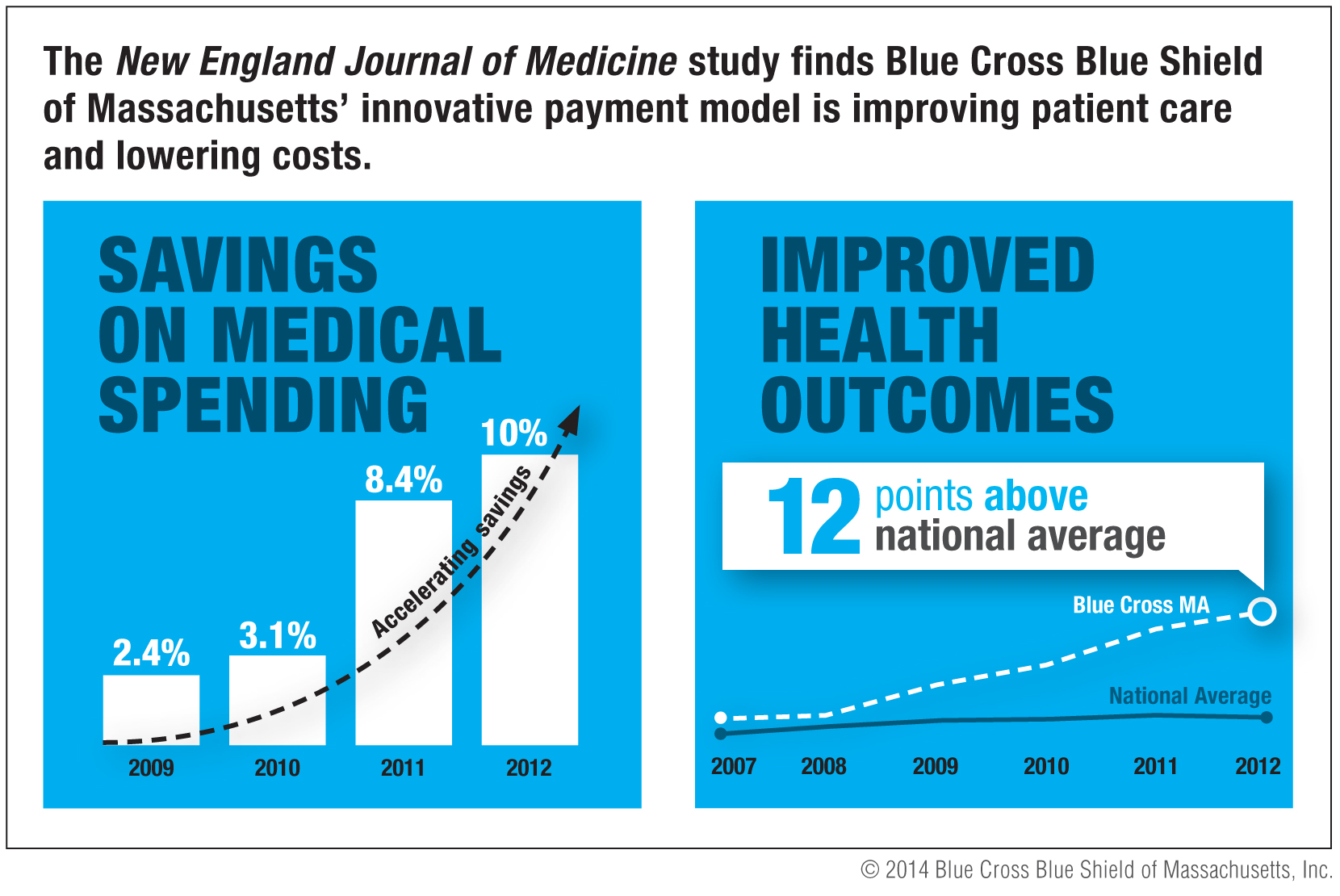
"Compared with similar populations in other states, Massachusetts AQC enrollees had lower spending growth and greater quality improvements after four years," the study authors concluded. The findings relative to the control group are important because they account for more general trends locally and nationally – showing that the AQC achieved savings over and above what was happening in the general environment.
Blue Cross CEO Credits Partnership with Physicians and Hospitals
"This rigorous evaluation of four years of data demonstrates that the AQC is achieving its twin goals of lower costs and better care for our members," said Andrew Dreyfus, President and CEO of Blue Cross. "These great results would not have been possible without the incredible effort, commitment and leadership of our physician and hospital partners."
Study Finds Quality of Patient Care Exceeded National Averages
The study also demonstrates significant quality improvements achieved under the AQC. While quality scores for Blue Cross members were on par with local and national averages prior to the AQC contract, the dramatic improvements in quality over the course of the contract show that members now receive quality of care that is significantly higher than national averages. These improvements include preventive care for healthy children and adults as well as improvements in the management of serious chronic illnesses.
"One of the pioneering features of the AQC was providers' willingness to accept accountability for the outcomes of care, and not just for the quality of what occurs in the office setting," said Dana Safran, ScD, Senior Vice President for Performance and Improvement at Blue Cross. "To be successful in managing outcomes, providers have to engage differently with patients and understand the things in their day-to-day lives that could get in the way of successfully managing their diabetes, hypertension or heart disease, and help patients develop ways to overcome those barriers. The results led to remarkable gains for individual patients and in population health – with thousands of patients with serious chronic illness now under good control, thereby avoiding the terrible and even deadly consequences that can occur when these conditions are not well controlled."
"The AQC has been transformative. It has allowed us to innovate because it enables us much more to think like a system rather than as an individual doctor or a small individual practice," said Leslie Sebba, MD, Medical Director, Northeast Physician Hospital Organization. "Most of the practices in a community like ours are two to five physicians at the most. We are able to introduce programs broadly across all the practices. The AQC allows us to do things more efficiently and gives us the resources to implement programs that would be very difficult for small practices to do."
Study Finds Significant Cost Savings
The study found the savings achieved by the AQC groups accelerated year by year. In the initial year, savings were approximately two percent compared to the control group, while by year four, the AQC groups saved 10 percent compared to control group. Savings were concentrated in the outpatient setting and explained by providers increasingly using lower cost settings and by reduced utilization, including discretionary procedures, imaging and testing.
"While it is true that medical trends were down across the country, by comparing the AQC to a rigorously designed control group, the study was able to show what the AQC was achieving in savings over and above these more general trends," added Dr. Safran. "To achieve significant quality and outcome improvements while significantly slowing spending growth – and to see this sustained and accelerated over a four year period – is a truly noteworthy achievement."
Harvard researchers discuss the results of their study on the AQC
About the AQC
Introduced in 2008, the AQC now includes 85 percent of the physicians and hospitals in the Blue Cross HMO network. It is an innovative way to pay for care that focuses on promoting quality and rewards positive health outcomes. It is a crucial component of Blue Cross' agenda to make quality health care affordable for its members and employer customers and is the predominant contract model between Blue Cross and its network physicians and hospitals. The alternative payment model fosters shared responsibility for both improving care and moderating the unsustainable rate of increase in health care costs. The AQC is currently one of the largest private payment reform initiatives in the United States. Read more about the AQC.
About Blue Cross Blue Shield of Massachusetts
Blue Cross Blue Shield of Massachusetts (www.bluecrossma.com) is a community-focused, tax-paying, not-for-profit health plan headquartered in Boston. We are the trusted health plan for more than 31,500 Massachusetts employers and are committed to working with others in a spirit of shared responsibility to make quality health care affordable. Consistent with our corporate promise to always put our 2.8 million members first, we are rated among the nation's best health plans for member satisfaction and quality. Connect with us on Facebook, Twitter, YouTube and LinkedIn.